
What goes wrong?
Compromising the sciatic nerve and its components by particular treatments, surgical interventions or injuries, limit day-to-day activities by affecting the lower extremity’s function. Musculoskeletal complications such as gait pattern deviations may occur i.e. drop foot, weak dorsi flexion and eversion, toe extensor difficulty, twisting ankle, tripping, sensory impairment to touch over the distal aspect of the leg and dorsum of the foot (Katirji & Wilbourn 1994, Vardi 2004, Viera et al. 2007, An et al. 2010) are signs of a compromised sciatic nerve, sciatica.
Typical manifestations of trauma to the sciatic nerve include; idiopathic palsy; postural habits; rapid weight loss; intrinsic or extrinsic nerve tumours; potential sciatic cross-over paths of propagation of intraneural cysts or extra neural compression by synovial cyst; soft tissue trauma; osseous mass or large fabella (LeGeyt & Ambrose 1998, Loredo et al. 1998, Spinner et al. 2003, Dellon 2005, Pokorny 2006, Spinner et al. 2007, Viera et al. 2007). Damage to the sciatic nerve could also be secondary; a fibular head fracture, knee dislocation, ankle sprains, surgical procedures such as hip replacement or intramuscular gluteal injection and application of skeletal traction or tight cast (LeGeyt & Ambrose 1998, Loredo et al. 1998, Spinner et al. 2003, Dellon 2005, Spinner et al. 2007, Viera et al. 2007). It is possible that with smaller individuals the sciatic nerve can be found in close proximity to the semitenidinosus and gracillis tendon and therefore in these circumstances may be prone to injury (Vardi 2004).
Diagnosis of ‘Sciatica’
Generally, an X-Ray or MRI will support, alongside a Manual Therapy assessment, the possible causes of sciatica. Sciatica is often described as mild to intense pain running down the posterior aspect of the leg(s). Sciatica is caused by compression of one or more of the 5 sets of nerve roots in the lower back, or compression on the sciatic nerve branch.
Six most common causes of sciatica;
- Trauma
- Piriformis syndrome – Anatomical anomalies (variations)
- Bulging or herniated intervertebral disc.
- Spondylolisthesis
- Lumbar spinal stenosis
- Spinal tumors
Piriformis Syndrome?
Piriformis syndrome is named when the pain caused by the piriformis muscle irritates the sciatic nerve. These various anatomical relationships of the piriformis muscle and the sciatic nerve have been reported for causing pseudo discogenic low back pain and symptoms, sometimes referred to as Piriformis Syndrome (Güvençer et al. 2008). Compression of the nerve by increased contracture of the piriformis muscle is thought to be the main cause (Babinski et al. 2003). It may be difficult to reliably diagnose (MRI and X-Rays are the Gold Standard i.e. the highest level ‘tool’ for diagnosing conditions) due to the lack of findings using these common methods.
Anatomical variations
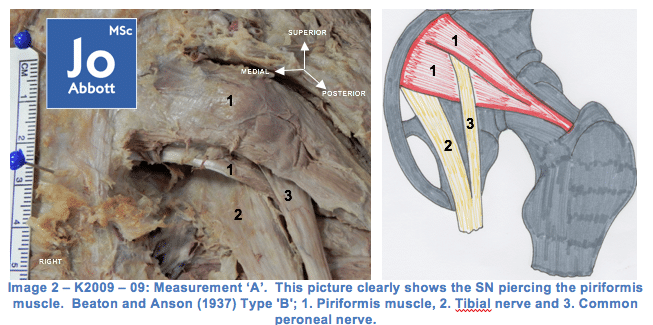
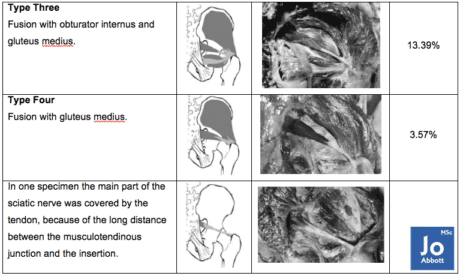
Beaton and Anson (1937) found six variations of anatomical relationship between the piriformis muscle and the sciatic nerve (see table below). Although the most common anatomical relationship between the piriformis and the sciatic nerve is the one the majority of us have learnt, we also really need to consider the other anatomical variabilities our Patient/Client may have.
THOUGHTS: Consider if you were a Type III and your Therapist wanted to ‘release‘ your piriformis with their elbow, do you think the experience is going to be a pleasant one? What if you had a Type II? How’d you think contracture of the piriformis may affect the nerve that bifurcates the muscle?
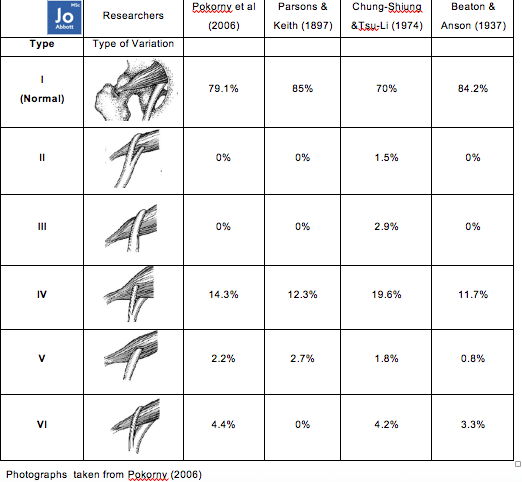
During my research of 24 cadavers (2010-2013) I documented finding Type I, Type IV, and Type V, and often finding variations of piriformis and sciatic nerve relationships between right and left-sides, of which embryology may dictate this variability. Within this study it may have been beneficial to look at the donors past medical history and to see if this bilateral asymmetry had any consequences on their daily activities? Unfortunately we do not get any information about how the donor lived in life and therefore are not able to make any inferences on any findings.
Other variations to consider
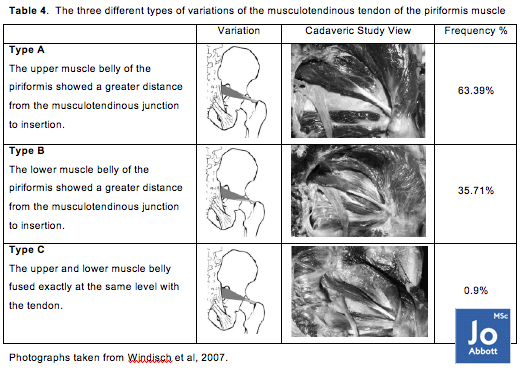
Increased tendon size? Does this mean this highly organized connective tissue joining muscle to bone, which is capable of resisting high tensile forces while transmitting forces from muscle to bone is needed in this deep hip external rotator?
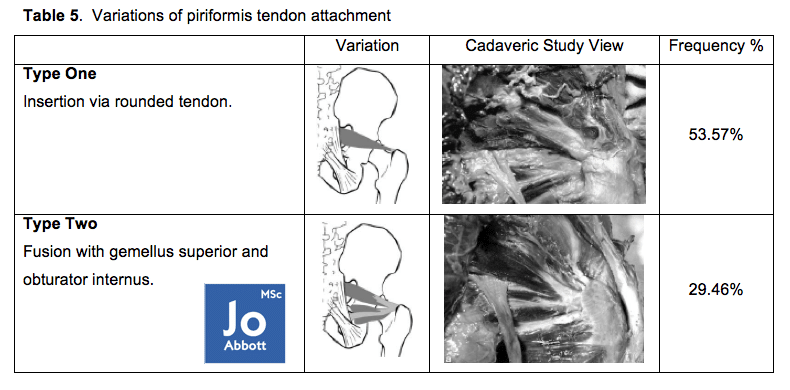
Fusion with the gemellus superior (GS) and obturator internus (OI)? Is it because we are doing more sitting and therefore more support is needed to help move the thigh outward (GS & OI), away from the midline of the body like getting out of a chair, whilst stabilising the hip joint (GS & OI)?
Fusion with the posterior fibres of gluteus medius? Why may we be evolving this variety?
Questions we should be asking.
On three cadavers I documented finding unilateral atrophied piriformis. Is this an anomaly of morphology so atypical it has never been found? Unfortunately, at the time, there were no studies supporting the comparison of piriformis between-limbs, between cadavers. Could this variability be underpinned by the ‘life’ the donor lived? For example; did the donor avoided weight-bearing on the atrophied-side due to pain? Did the donor have a hobby or career that was dominant on one-side of the lower body and therefore hypertrophied the piriformis? Unfortunately, we are not given the ‘life’ of the donor to make any inferences of their individual anatomical findings which ultimately could be the healthcare investigative ‘signature’ to progress musculoskeletal sciences.
Most common treatments for sciatica
- NSAIDS
- Prescription muscle relaxants to ease muscle spasms
- Antidepressants for chronic low back pain
- Prescription pain medications for more severe pain
- In some cases, a steroid medication is injected into the space around the spinal nerve. Research suggests these injections have a modest effect when irritation is caused by pressure from a herniated, or ruptured, disc.
Questions we should be asking
- Are NSAIDS the best option for our Patient/Clients? Is their Gut Health optimal? An easy way to know is to ask if they have any food intolerances. If they are not aware, to this detail, about their health – order a stool sample or complete a Mineral Test.
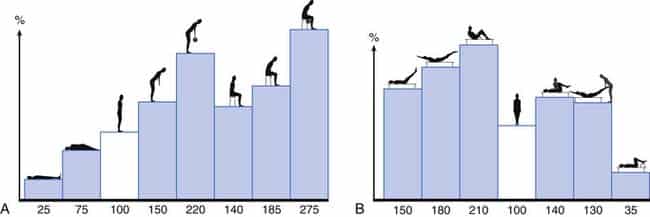
- Steroid Injections are chemicals, often hormones, that your body makes naturally. They help your organs, tissues, and cells do their jobs. Corticosteroids are medicines that quickly fight inflammation in your body. Cortisol keeps your immune system from making substances that cause inflammation. Often steroids are used either directly in to the sciatic nerve or in to the lumbar spine to reduce pain. But do steroid injections ever get to the cause of the problem? Do they ever find and re-organise the driver that caused the pain cycle? How good are these injections if the aftercare needed is never discussed with the Patient? An example would be epidural injections for symptoms of sciatica believed to be coming from the lumbar discs. For the anti-inflammation to work do we not need to remove the driver? Maybe the driver was consistent poor posture? The graph below demonstrates the percentage of spinal load at the third lumbar disc (data taken as intradiscal pressure) that occurs in various lumbopelvic hip positions. The safe zone of ‘reduced relative risk’ for loading the spine is 0-100%, beyond this and the risk for injury increases, more-so in a de-conditioned spine. It’s worth considering most people with low back pain who are in need of a steroid injection are commonly de-conditioned due to the limitations the symptoms have on daily life. The best outcome post-steroid injection would be to avoid adding any loads above 100% for a couple of days – allowing the steroid to do the work it has been prescribed to do. Unfortunately, there is no research to date on ‘the success rates of steroidal injections followed with CBT training bringing awareness to reduce load on the spine post-treatment’ because it has never conducted. For me, it’s a big part of whether the intervention will succeed or not.
Following Blog: Case Report
- Exploring the common conversation and reporting of a real-life Case Study.
- Looking at what may underpin the Case Studies symptoms.
- What we may want to consider as a Manual Therapist/Personal Trainer/Movement Specialist?
-
There are so many mechanisms involved in squatting, some of these mechanisms are fundamental to the human design, others blow off the cobwebs and allow us to keep moving safely and efficiently. Reducing squatting exposes the joints to premature aging; knees, hips, ankles, spine, and pelvis.
-
Thumb joint corrects foot pain! Seriously?
I know, crazy right? I must be mistaken? It has to be some kind of black magic? I'm pain-free because of some other factor? It must be psychosomatic?To be honest, I have heard it all now. What's important? My wrist is pain-free enabling me to get back to a normal life after 2 years of pain!


0 responses on "The Sciatic Nerve, it's Anatomy, that will make you understand it's Pain 3/12"