
Bigger Picture Stuff
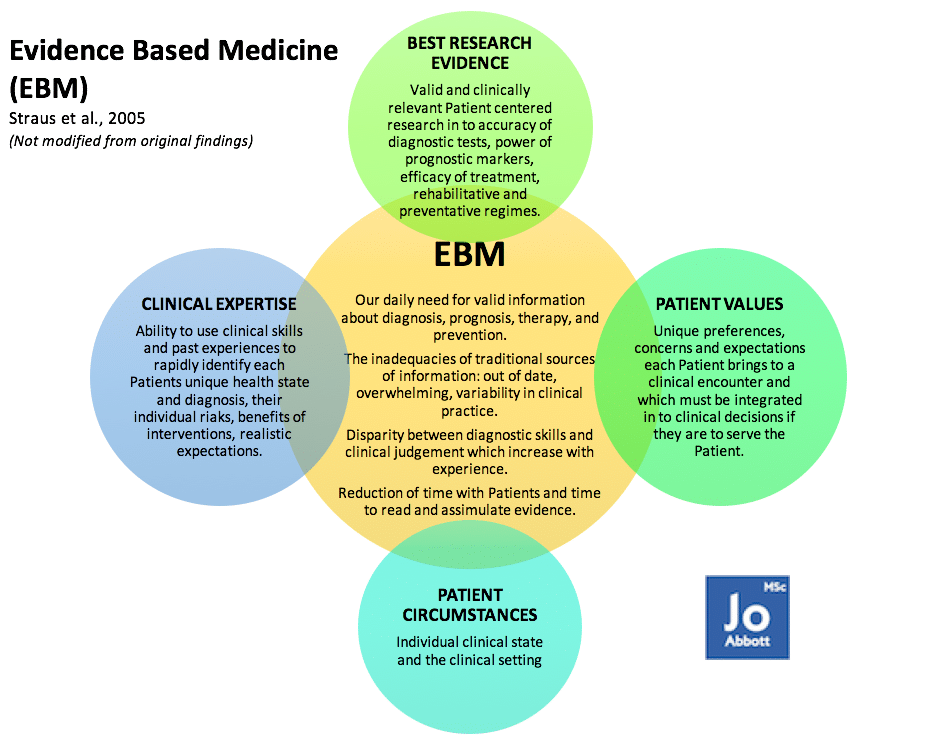
Full Patient/Client History is nothing to be taken likely when exploring sciatica – it is a quarter (see image below) of your initial exploratory investigations in to why the person is sitting in front of you seeking your help and support. Besides, have you ever met a Patient/Client (P/C) who doesn’t want to tell you about their woe’s? About the things that are bothering them? What causes their pain? What they are no longer able to do? What their goals are? And why they sought out your help? Taking good P/C history is the beginning of your journey together. This drives the ability to; set specific goals for you both: maximising outcomes in minimum time; and ensure you explore/define/question parts of their history allowing you to triangulate (a powerful technique that facilitates validation of data through cross verification from two or more sources) your theory (hypothesis). This is hypothetical deductive reasoning.
Hypothetical Deductive Reasoning (Piaget)
Is the ability to perform abstract mental operations, and to become more scientific and logical in the way you approach problems. Piaget called this methodical, scientific approach to problem-solving, and is one of the most basic methods common to all scientific disciplines including biology, physics, and chemistry.
To understand the reasons why a P/C is not performing optimally (movement, exercising, socialising, eating, employment, etc) is generally within their personal story – remember, we are in this industry to help/support the person who has seeked us out. This is not about us, it never has been.
This all might sound scientific or extravagant, but it is your duty of care to support P/C’s that are paying for your services to guide them to better health and well being. I’m not discussing ‘cults‘ nor my ‘belief systems‘ (I’m an unbiased scientist!) on what I think is right for the P/C. The information I give you is EBM which supports you being the best you can be, whilst giving the P/C the best support proven by years of research and clinical practice.
Exploring in vivo Sciatica Case Studies
The following Case Studies have been supplied by a Private Facebook Group. Thank you guys for sharing. All Case’s have been diagnosed with Sciatica, each with a individual’s story of events and symptoms. The name “sciatic” came via Latin from the Greek “ischiadikos” which means “subject to trouble in the hips or loins.”
Case Study 1
Event that provoked Sciatica: April 2015 lifting heavy weights and squeezing gluteals causing a pelvic tilt.
Symptoms: “It felt like an elastic band twanging across my lower back. It took 2/3 days before the full severity of what I had done kicked in. I couldn’t stand or move for 10 days. I had severe pain in my back, down my left leg, in my hamstring, calf and outside of my foot.”
Current Symptoms: Although my symptoms have improved I still suffer from numbness to the outside of my foot and occasional hamstring pain. My sport of Olympic Weightlifting has helped in my recovery although I have to be cautious with my movements.
Diagnosis: L4/L5 and L5/S1 bulging discs.
Treatment: Physiotherapy; no change to symptoms. Surgery offered for next step to improve symptoms, of which this has been declined.
Lifestyle
Drives a manual HGV for long hours which aggravates symptoms.
Applying hypothetical deductive reasoning:
- The P/C’s story suggests the disc bulge’s may have been on the left-side of his intervertebral discs at L4/L5 and L5/S1, which may explain the neuropathy in his lower left leg, hamstring, calf, and foot.

- Current symptoms suggest the tibial nerve remains compromised at L5/S1 (Follow the orange tibial nerve from the lumbar plexus (L4, L5, S1, S2, & S3) down to the foot). Tibial nerve supplies the foot and hamstrings. Pain remaining in the hamstrings suggests a radiculopathy (compression of the nerves as they exit the spine, an irritation of or injury to a nerve root that causes pain).
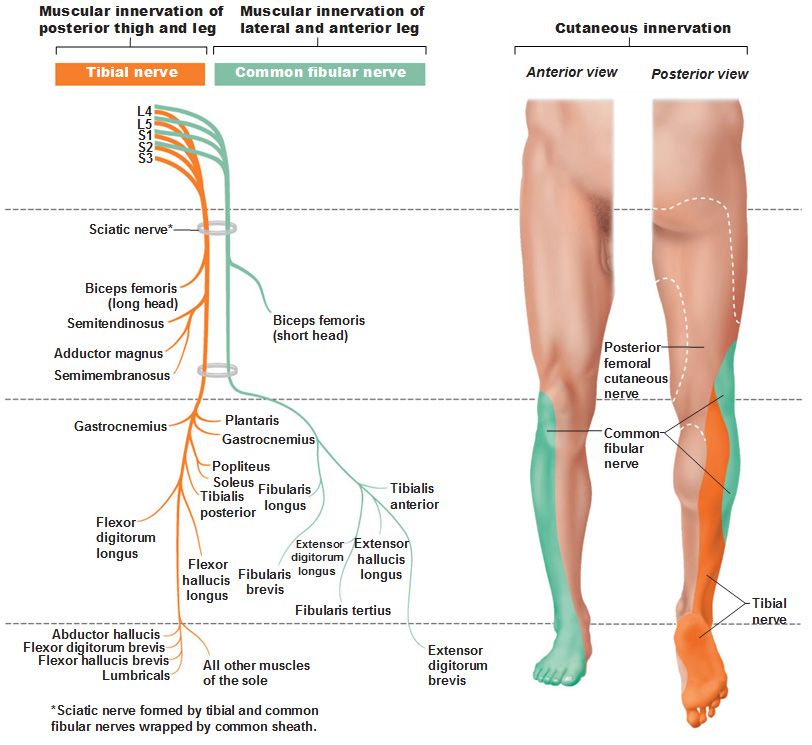
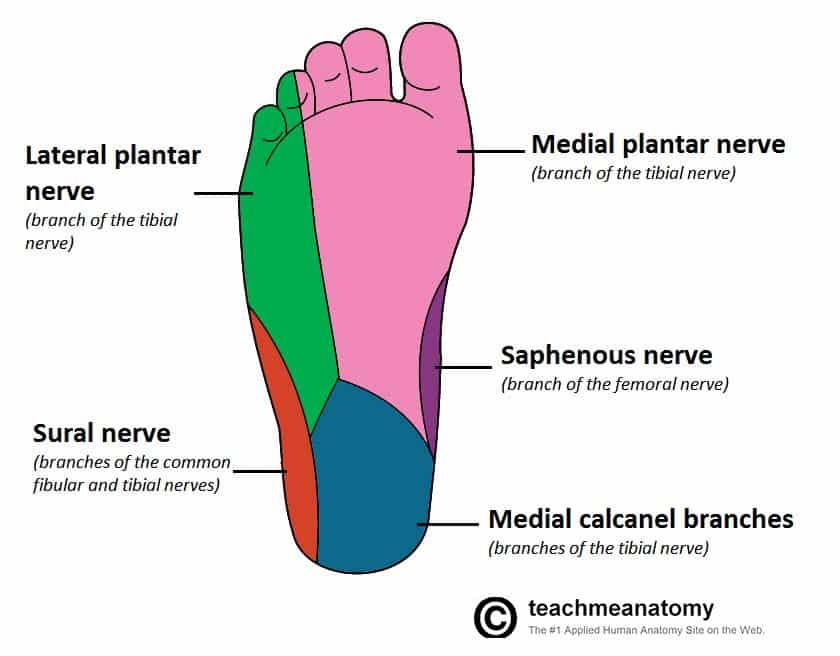
- With numbness, suggesting a neuropathy (disease or dysfunction of one or more peripheral nerves, typically causing numbness or weakness), on the outside of the foot suggests reduced sensitivity of the dermatomes in this area. A dermatome is an area of skin that is mainly supplied by a single spinal nerve, in this case S1 tibial nerve (see image below).
- Further triangulation of specific tools would add to this diagnosis.
- “Driving a manual HGV aggravates symptoms” – why would this be? Posture? Climbing in and out of the HGV? Lack of vibration dampening in the seat mechanisms? Mechanisms of driving i.e. legs on pedals and arms on steering wheel causing a stretch on the CNS? Whats is this P/C relative risk? i.e. is he sat in a non-optimal position in his lumbar spine and pelvis which is causing the symptoms to get worse? Does he have missing teeth, in particular his molars? Does he have a head forwards posture which is adding increased load to the spinal column? These can only be answered in the P/C History taking process and assessment session.
Fear of failure?
Don’t be – you are missing imperative opportunities for yourself and the P/C. Build on the hypothesis, then go test it! Were you successful? i.e. did it improve the persons symptoms? No? Good, because you are about to go through some valuable learning that no Course can give you! The biggest steps in discovery have been due to hundreds, often thousands, of failures. Failure allows you to learn and go back to your hypothetical deductive reasoning. James Dyson (Dyson Vacuum) failed over 4,000 times before he succeeded!
Ethics
Ethically, if you believe, through hypothetical deductive reasoning, that you gave the P/C the best advice/treatment/exercises that you surmised in your session with them (and you can justify what you did): then you gave the best care to that P/C available to you at that time. If their symptoms worsen, you go back to the white board and start again, or maybe seek help and support from other professionals.
Next weeks Blog:
- Strongman Competition Case Study
- Muscle Mechanics (Tissue Mechanics)
- Why stretching may make something that feel’s tight, worse.
-
There are so many mechanisms involved in squatting, some of these mechanisms are fundamental to the human design, others blow off the cobwebs and allow us to keep moving safely and efficiently. Reducing squatting exposes the joints to premature aging; knees, hips, ankles, spine, and pelvis.
-
Thumb joint corrects foot pain! Seriously?
I know, crazy right? I must be mistaken? It has to be some kind of black magic? I'm pain-free because of some other factor? It must be psychosomatic?To be honest, I have heard it all now. What's important? My wrist is pain-free enabling me to get back to a normal life after 2 years of pain!


0 responses on "Behind the Scenes of a Patient with Sciatica 4/12"